We’ve reached the final chapter in our journey through the twelve senses—a journey that goes well beyond the sights, sounds, and textures most of us first think of. For parents of neurodiverse children, understanding these less obvious senses is the key to unlocking new ways to support self-awareness, emotional regulation, and daily well-being.
In Part 1, we covered the classic five senses. In Part 2, we explored the “hidden” senses of balance and body position. Now, we’re focusing on the five remaining senses, often called the “internal” or “interoceptive” senses. These play a vital role in everything from morning routines to how your child interprets their own emotions.
This article will help you recognize the signs, explain these senses to your child, and offer practical strategies and family routines to support your neurodiverse child as they grow.
Internal Body Signals (Interoception)
Interoception is the sense that helps us notice and make sense of our internal states—when we’re hungry, thirsty, tired, anxious, excited, or need to use the bathroom. You can think of it as your body’s built-in communication system, sending messages all day long.
For neurodiverse children, interoception can be a major challenge:
- Hyposensitivity: A child may not feel that they are hungry until they are irritable or even feeling unwell, or might not notice a full bladder until an accident occurs. They might play through a scraped knee without realization, missing early signals of injury or discomfort.
- Hypersensitivity: Another child may be acutely aware of every gurgle, flutter, or quickened heartbeat. This can create anxiety and even panic, as minor sensations—like a slightly tight stomach or a skipped heartbeat—feel overwhelming.
Explaining Interoception to Your Child
“Your body has a special messenger that sends you quiet notes. Sometimes, it whispers, ‘You’re getting thirsty’ or ‘It’s time to use the bathroom!’ For some people, those messages are very quiet, and we have to learn to listen for them together.”
Tips and Activities
- Routine Body Scans: Make it a habit to pause several times a day and model a quick self-check. Ask yourself aloud, “Hmm, is my throat dry? Does my tummy feel empty?” This helps your child build self-monitoring skills.
- Feelings and Body Charts: Pair feelings with physical states. Make or print a chart with cartoon faces and body parts (“When I’m hungry, my tummy growls”; “When I’m anxious, my hands get sweaty”).
- Story Time with a Twist: Read stories together and pause to wonder aloud how a character might feel inside their body. “Do you think Frog’s heart is beating fast because he’s excited?”
- Use Timers or Schedules: Some children benefit from routines—offer water breaks and bathroom reminders on a visual schedule, especially during high-focus activities or when away from home.
- Mindfulness and Movement: Simple yoga stretches, breathing exercises, or “freeze dance” games help children tune in to their heart rate and breath. Practice noticing how these change after activity, and talk about what those signals mean.
Temperature (Thermoception)
Thermoception is your body’s ability to sense heat and cold through the skin and internal sensors. It’s a silent safety feature: it helps us know when to seek shelter, add layers, or back away from a hot stove. But this sense is easily overlooked until it becomes a struggle.
How It Shows Up in Neurodiverse Kids
- Hyposensitivity: Maybe your child doesn’t mind playing outside in freezing weather or refuses to wear a jacket. Or maybe they jump right into a hot bath without complaint—but later show red, irritated skin.
- Hypersensitivity: For some, warm air from a heater feels like a blast furnace, and the subtlest change in room temperature can trigger distress. A humid summer day may be unbearable, while even a light breeze can be “too cold.”
Explaining Thermoception to Your Child
“Your skin is covered in invisible thermometers that tell your brain if you’re warm, cool, or just right. Sometimes, these thermometers shout too loudly or whisper so softly we can’t hear them. It’s okay to ask for help if you feel comfortable or uncomfortable.”
Tips and Activities
- Thermoception Exploration Laboratory: Fill two bowls with safe, noticeably different water temperatures (not hot enough to scald, and not ice cold). Let your child touch or play with small plastic toys in the water, and talk about how each water feels.
- Temperature Guessing Game: Use fabric swatches kept at different temperatures (outdoors, near a vent, under a warm light) and have a guessing game with eyes closed.
- Weather-Dependent Dressing: Before heading outside, check the forecast together. Place choices on the bed—short sleeves, sweaters, jackets—and let your child pick what feels right, guiding them gently if needed.
- Setting the Environment: Allow your child a say in room temperature—maybe an extra blanket for movie time, or a portable fan for bedtime. Empowering small adjustments can help your child self-advocate.
- Safe Exploration: Use a washable marker to note which faucet is hot or cold; practice hand-washing with both. Remind them never to test heat with their whole hand—always with a carefully running tap or adult assistance.
Pain (Nociception)
Nociception is the sense that protects us from injury. It tells us when something is sharp, burning, pinching, or otherwise harmful to our body. But it isn’t one-size-fits-all.
How It Shows Up in Neurodiverse Kids
- High Pain Threshold: Your child takes a tumble and barely notices the cut on their knee—sometimes even playing with broken skin or missing the need for first aid. This can be risky, as injuries may go untreated.
- Low Pain Threshold: Conversely, a gentle pressure from a seatbelt, a tiny scratch, or an insect bite can feel excruciating, making routine activities challenging.
- Emotional Pain Sensitivity: Some children also process social or emotional pain more intensely, which can be another form of “nociception.”
Explaining Nociception to Your Child
“Pain is your body’s alarm system. It’s like a smoke detector that shouts ‘Ouch!’ when something isn’t safe. Some smoke detectors are sensitive and go off at little things, while others are really quiet. If yours is shouting or whispering, it’s always okay to ask for help or comfort.”
Tips and Activities
- Build a “Boo-Boo Toolkit”: Fill a small box with age-appropriate supplies—fun bandages, a cool pack, favorite stickers, and a comfort item. Practice using it when real or pretend injuries occur.
- Describe and Rate Pain: Teach your child to communicate about pain by using tools like a rainbow of faces (smiling to crying) or a number scale. “Is your ouch a 1 like a tiny pebble, or a 5 like a big rock?”
- Role-Playing Helpfulness: Use dolls or action figures to act out getting hurt and treating “ouchies” together. This helps a child become comfortable reporting their own injuries.
- Body Map Game: Draw a simple outline of a person and use it to mark areas where your child notices pain or discomfort. This boosts awareness and gives you both language to discuss what happened.
- Comfort Rituals: Create soothing routines for pain—gentle music, holding hands, snuggling, or deep breaths—so your child knows they will be cared for, no matter the level of pain.
Time and Direction
Time and spatial orientation aren’t the same as hunger or temperature, but they are “internal” senses that help us move confidently through daily routines, social situations, and new environments.
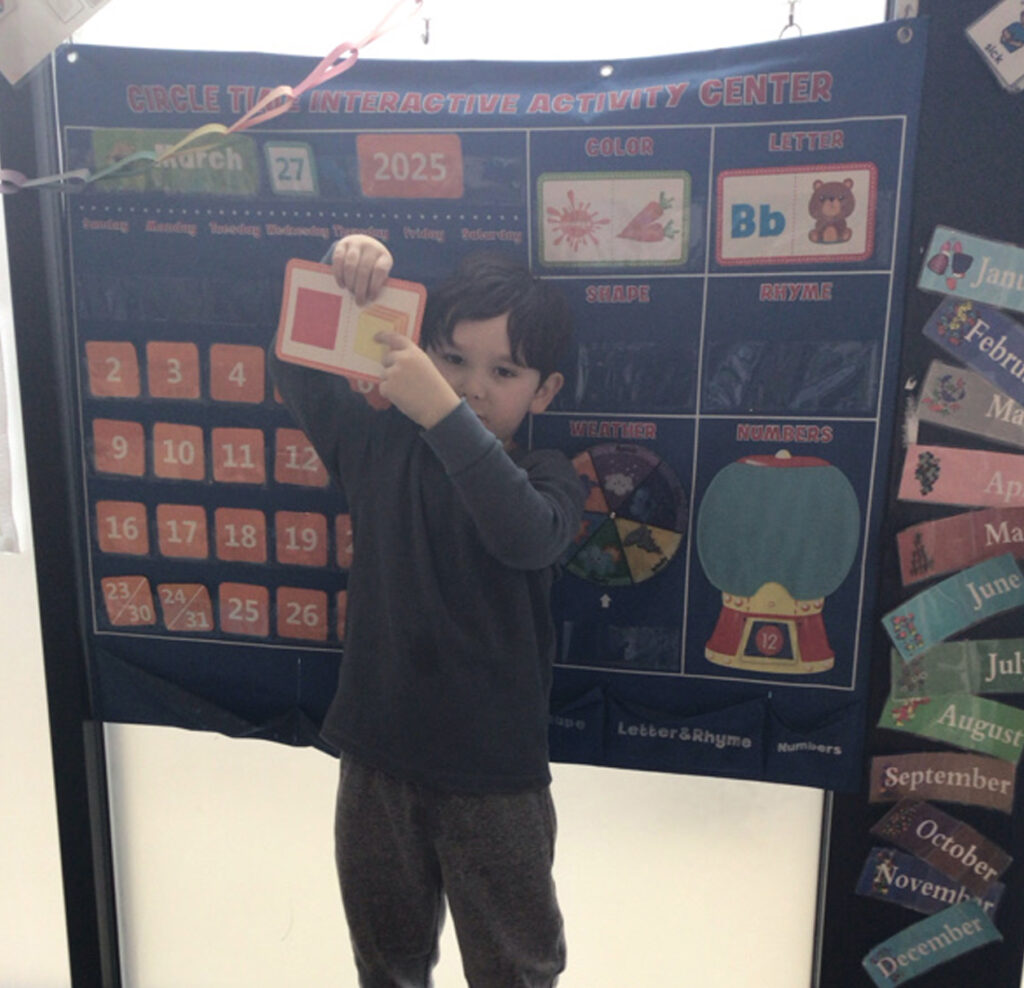
Chronoception (The Sense of Time)
Chronoception is our internal clock—it helps us sense how much time has passed and lets us judge how long a task or break will take. Many neurodiverse children experience “time blindness”: the struggle to judge minutes, wait for transitions, or even understand when it’s time to stop or start an activity.
Explaining Chronoception to Your Child
“Your brain has a special clock inside, but sometimes it runs too fast or too slow. A timer or countdown clock helps your brain know when things will start and stop, so surprises are smaller and changes are easier.”
Tips and Activities
- Timelines and Visual Schedules: Use strips of paper or picture cards for each step in a routine (“wake up,” “get dressed,” “eat breakfast,” “brush teeth,” “leave for school”). Check each off as you go.
- Timers for Everything: Physical timers (sand, egg, or digital) or timer apps give instant feedback. Practice using them for fun (two-minute jumping contests, quick craft projects, “beat the timer” games).
- Countdown Rituals: Announce upcoming transitions with a “5-minute warning,” and again at “2 minutes,” then a final countdown.
- Time Talks: At bedtime, discuss the next day’s schedule. Use analogies—“When the big hand is on the 12, it’s time for…,” “This show is as long as a car ride to Grandma’s.”
- Waiting Game: Practice waiting with a tangible reward, like a token jar or sticker board—“If we wait with calm bodies for five minutes, you can pick the next story.”
- Calendar Awareness: For older children, mark special days and color-code the calendar together. Counting down visually helps with anticipation and decreases surprise anxiety.
Magnetoception (Sense of Direction and Space)
Magnetoception is the sense that helps with spatial orientation—finding north, knowing left from right, and understanding where our body is in relation to objects, rooms, and larger environments. While it’s thought to be especially strong in birds and some animals, humans rely on a subtle version to navigate homes, schools, and the world.
Signs in Neurodiverse Children
- Challenges noticing or remembering directions (“Oops! I forgot where the bathroom is.”)
- Trouble following multi-step tasks, especially ones involving movement through space (“Put your backpack in the hall, and then wash your hands.”)
- Getting lost or disoriented in new places.
- Confusion between left and right well past early childhood.
How to Explain Magnetoception to Your Child
“Your brain has a tiny, invisible compass that helps you find your way. Sometimes it feels confused, and that’s okay. We can use tricks, maps, or practice games to help your inner compass get stronger.”
Practical Tips and Activities
- Map-Making Adventure: Draw a simple map of your home or local playground and take turns finding different “treasure” locations. Play “hot and cold” while searching to build directional confidence.
- Landmark Learning: Choose distinct features in your house or neighborhood as visual “anchors”—“The blue door means it’s time to turn left,” “The clock is next to the kitchen.”
- Step-by-Step Navigation: Play “Simon Says”-style games with directions. “Turn right at the chair, then hop forward three steps, then turn left.”
- Directional Songs and Dances: Use music and movement—like “The Hokey Pokey”—to reinforce left/right and forward/backward concepts in a playful way.
- Routine Review: After outings, ask questions to help reinforce spatial memory. “How many turns to get from the car to your classroom? What do you see along the way?”
- Explore Safe Spaces Together: Let your child lead in a familiar store or park. Even if they get turned around, use it as a calm teaching moment—“Let’s find our way back by spotting the red slide!”
Embracing All Twelve Senses
Knowledge is a bridge to connection. By understanding and supporting the full range of your child’s senses—including the most invisible ones—you honor their entire experience. You build resilience, give them language for self-advocacy, and unlock new ways for them to feel safe in their bodies and empowered in the world.
There’s no single right answer for every child, and needs will shift over time. Stay curious, trust what you notice, and collaborate with teachers, occupational therapists, and—most of all—your child.
Thank you for joining us for this journey!

Blue Bird Day—the first therapeutic preschool and kindergarten program in the nation—fosters socialization, sensory regulation, and pre-academic learning in children ages 2-7 years. Our compassionate therapists practice a relationship-based and family-centered approach, provide parent training, and collaborate on goals and individualized intensive treatment plans for your child.
We believe in a collaborative and multi-disciplinary team approach to therapy. A team of occupational therapists, speech-language pathologists, dietitians, developmental therapists, behavioral therapists, physical therapists, and therapeutic assistants are created for each child to ensure child and family are fully supported and the best possible results are achieved.
Options for individualized, group and virtual therapy sessions are available as well.
Want to learn more or you have a specific question? Feel free to connect with us here!