Does your child cover their ears in the grocery store? Refuse to wear certain textures? Crave crashing into furniture? Do they ignore you after you call their name many times?
These responses can be very frustrating, but if you look deeper, they tell you something important about how your child’s nervous system receives and is processing information. Sensory processing refers to the way our brain organizes sensations from our body and environment and then processes the input.
For some children, this process works differently, creating experiences that some people might find puzzling or annoying. Their reactions are not tantrums or defiance. They are genuine, physiological responses to sensory input.
No sensory experience is wrong. Brains simply process information differently, and that variation is part of being a human being.
We are all wired a little bit differently. Some people have sharper senses, others need more intense input to register sensation, while others seem off in their own world. All are valid ways of experiencing life.
What Is Sensory Processing Disorder?
Sensory Processing Disorder, often called SPD, describes a neurological difference in how the brain interprets sensory information. When someone has SPD, their nervous system struggles to receive, organize, or respond to sensory input in a way that allows smooth daily functioning.
Many people confuse Sensory Processing Disorder with being “too sensitive” or “too picky.” That misses the reality. SPD is not about preference or personality. It reflects genuine differences in neurological wiring. The brain either amplifies certain sensations, dampens them, or has trouble making sense of them at all.
SPD shows up in different forms. Some children have hypersensitivity, where sensations feel overwhelming or even painful. A tag in a shirt becomes unbearable. Background noise drowns out conversation. Bright lights cause physical discomfort.
Other children experience hyposensitivity. They need more intense input to register sensation. They might not notice when they’re hurt. They seek out strong flavors, crash into things, or seem unaware of their body in space.
Then there are sensory seekers who actively crave intense sensory experiences. They want to touch everything, make loud noises, spin constantly, or chew on objects. Their nervous system needs more input to feel regulated.
Many children show mixed profiles. They might be hypersensitive to sound but hyposensitive to touch. They could seek movement but avoid certain textures. The combinations are endless because every nervous system is unique.
Signs and Symptoms Across Ages
Infants with sensory differences might arch away from being held, startle easily at sounds, or struggle to settle despite being fed and changed. They may cry intensely during diaper changes or hate having their face wiped. Some babies do the opposite, seeming unusually calm or not responding much to stimulation.
Toddlers often show clearer patterns. They might refuse entire categories of food based on texture. They have meltdowns over getting dressed. They run away from hand dryers or vacuum cleaners. Or they constantly seek movement, never seeming to tire from physical activity.
School-age children face new challenges. The sensory demands of classrooms can be intense. Fluorescent lights, crowded hallways, cafeteria noise, and the expectation to sit still all day create stress. Some children avoid messy activities like finger painting or sand play. Others have trouble with handwriting because the pencil feels wrong or they cannot judge how much pressure to use.
Teens often develop coping strategies but still struggle. Social situations become more complex. They might avoid school dances because of the music volume or decline invitations because they cannot handle certain restaurant environments. Some withdraw socially to avoid sensory overload. Others push through but pay the price with exhaustion or meltdowns at home.
For autistic children, sensory differences are often more pronounced. They might have intense reactions to specific triggers and need clear, consistent strategies to manage. ADHD children frequently seek sensory input through movement and touch. They fidget, rock, or need to touch objects while thinking.
The key difference between typical sensory preferences and SPD lies in impact. Everyone has sensory likes and dislikes. SPD interferes with daily activities, relationships, or quality of life. A child who prefers soft clothes is different from one who cannot get dressed without crying. A kid who dislikes loud movies is different from one who cannot enter a birthday party because of the noise level.
The Neurodiverse Parent Perspective
When you share neurological traits with your child, you bring unique strengths to parenting. You often recognize sensory triggers before anyone else does. You know what a sensory meltdown looks like from the inside. You understand that sometimes the body just needs deep pressure or total darkness or absolute silence.
This insight helps you respond with empathy rather than frustration. When your child melts down over a seam in their sock, you do not dismiss it as drama. You remember how that feels. You can validate their experience genuinely because you know it is real.
You might also notice patterns between your sensory needs and theirs. You both struggle with sudden loud noises. You share an aversion to certain food textures or a need for quiet time after social events. These connections help you predict challenges and plan.
However, shared traits can also create challenges. Your child might need loud music to focus while you need silence. They might crave constant physical contact when you need space. One person’s regulation strategy becomes another’s sensory nightmare.
These conflicts require honest communication and creative solutions. You might use noise-canceling headphones while your child listens to music. You could establish “touch times” and “space times” throughout the day. The goal is to meet everyone’s needs without anyone feeling wrong or burdensome.
Neurodiverse parents also bring permission for differences. You model accepting your own sensory needs, which teaches your child to accept theirs. When you leave a party early because of sensory overload, you show them that self-care matters more than social expectations. When you say “I need quiet right now” without shame, you demonstrate healthy boundary-setting.
The Eight Sensory Systems
Most people learn about five senses in school, but humans process eight types of sensory information.
The tactile system oversees touch. It includes texture, temperature, pressure, and pain. Children with tactile differences might hate light touch but crave deep pressure. They could avoid messy play or constantly touch everything around them.
The auditory system processes sound. This includes volume, pitch, and the ability to filter background noise from essential information. Some children hear everything at once, making it hard to focus on one voice or sound. Others seem not to hear their name being called.
The visual system involves sight. This means more than seeing clearly. It includes processing visual information, handling different light levels, and filtering competing visual stimuli. Bright lights, busy patterns, or fluorescent bulbs can overwhelm some children. Others might not notice visual details or have trouble tracking moving objects.
The gustatory system covers taste. Children might be extremely fussy eaters, not because they are stubborn, but because their gustatory system makes certain flavors overwhelming. Some seek out intense flavors while others stick to bland foods.
The olfactory system handles smell. Strong scents that others barely notice can cause nausea or headaches for sensitive children. Some cannot tolerate perfumes, cleaning products, or even certain foods cooking. Others might not notice strong odors at all.
The vestibular system monitors movement, balance, and spatial orientation. It tells us where our body is in space and whether we are moving or still. Children who seek vestibular input might spin, swing, or jump constantly. Those who are sensitive might fear playground equipment or dislike being tipped backwards.
The proprioceptive system provides information about body position and movement through muscles and joints. It helps us know how much force to use and where our body parts are without looking. Children who need proprioceptive input might crash into things, jump heavily, or seek tight hugs. Those with poor proprioception might seem clumsy or use too much or too little force.
Interoception is the eighth and often overlooked sense. It registers internal body signals like hunger, thirst, pain, temperature, need to use the bathroom, and emotions. Children with interoceptive differences might not realize they are hungry until they are starving or not notice they need the bathroom until it is urgent. They might have trouble identifying emotions because the physical sensations are unclear.

Practical Strategies for Home
Creating a sensory-friendly home starts with observation. Notice what helps your child regulate and what causes distress. Keep notes about patterns. Does morning light bother them? Do they focus better after jumping on the trampoline? Does background music help or hinder?
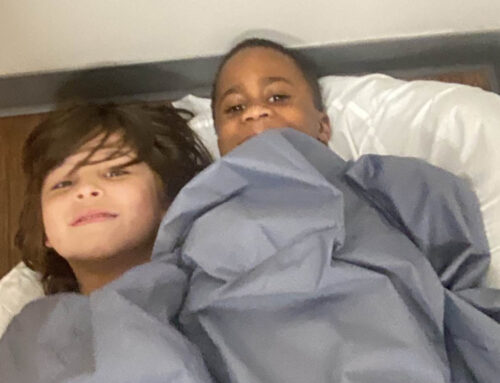
Build a sensory toolkit based on your child’s specific needs. For tactile seekers, include items like therapy putty, textured balls, or fidget toys. For those who need calming input, try weighted blankets, soft fabrics, or gentle lotions. Auditory tools might include noise-canceling headphones, white noise machines, or playlists of preferred sounds.
Movement tools matter too. A small trampoline, yoga ball, or crash pad can provide vestibular and proprioceptive input. Even a designated space for safe crashing helps children get the input they need.
Environmental adjustments make daily life easier. Use dimmer switches or lamps instead of overhead lights. Create quiet zones where anyone can retreat when overwhelmed. Consider which sounds happen in your home and whether some could be eliminated or reduced. Even slight changes like switching to unscented laundry detergent can help sensitive children.
Routines provide predictability, which reduces stress. When children know what to expect, they can prepare mentally for sensory challenges. Morning and bedtime routines especially benefit from consistency. Include sensory activities that help with transitions, like jumping jacks before school or a warm bath before bed.
Co-regulation means helping another person regulate their nervous system through your calm presence. When your child feels overwhelmed, your regulated state can help them find their way back to calm. This might look like sitting quietly nearby, offering deep pressure through a hug, or modeling slow breathing. The key is to stay regulated yourself, which is easier said than done when you are also neurodiverse.
Transitions between activities or locations often trigger meltdowns. Give warnings before changes. Use timers, countdowns, or visual schedules. Allow extra time for transitions so children can mentally prepare and physically move at their own pace.
When meltdowns happen, focus on safety and co-regulation rather than consequences. A meltdown is not a behavioral choice. It is a nervous system crisis. Dim lights, reduce noise, offer comfort items, and give space if needed. Talk about what happened later when everyone is calm.
School and Community Challenges
Teachers need to understand your child’s sensory needs to support them effectively. Share specific information. Instead of saying “my child is sensitive,” explain “loud noises cause physical pain, so please allow them to use noise-reducing headphones during assemblies.”
Provide examples of what works at home. If your child focuses better while moving, mention that. If they need breaks in a quiet space, say so. Teachers appreciate concrete suggestions more than general requests.
Useful accommodation might include preferential seating away from windows or noisy areas, permission to use fidget tools, scheduled movement breaks, alternative lighting, or a quiet space for regulating. Some children benefit from modified expectations for messy activities or different options for demonstrating learning.
Advocacy requires energy, and neurodiverse parents often have limited reserves. Pick your battles. Focus on accommodations that make the biggest difference. Build relationships with teachers through positive interactions, not just requests. Many educators genuinely want to help but need specific guidance.
Help your child learn to communicate their sensory needs. Young children can learn phrases like “too loud” or “need break.” Older kids can understand their sensory profile and request specific support. Self-advocacy skills serve them throughout life.
Community outings require planning. Preview new environments when possible. Bring sensory tools in a bag. Identify quiet spots or exits. Set realistic expectations. Leaving early is not failure. It is good sensory self-care.
Some families create cards explaining their child’s need to hand to confused strangers. Others simply leave situations without explanation. Both approaches are valid. Your family’s comfort matters most.
When to Seek Professional Support
Occupational therapists specialize in sensory processing. They assess how sensory differences impact daily functioning and create individualized strategies. Not every child with sensory differences needs therapy, but OT helps when sensory challenges significantly interfere with life.
Consider evaluation if your child cannot participate in typical activities because of sensory issues. If dressing takes an hour every morning or they cannot eat enough variety to stay healthy or they are so overwhelmed they cannot learn at school, professional support may be needed.
An OT evaluation typically includes interviews with parents, observation of the child, and standardized assessments. The therapist looks at how all sensory systems function and how they impact daily activities. They identify specific areas of difficulty and strength.
Therapy sessions might look like play, but they have specific goals. Activities are designed to help the nervous system process sensory information more efficiently. This might include swinging, climbing, playing with different textures, or practicing specific tasks while receiving sensory input.
The best OT works collaboratively with families. They teach you strategies to use at home and help you understand your child’s sensory system. Therapy is not about making children “normal.” It’s about giving them tools to function more comfortably in their body and environment.
Signs that additional support might help include intense distress over sensory experiences, inability to calm after sensory input, avoiding so many things that daily life is limited, or seeking sensory input in ways that are unsafe. Trust your instinct. You know your child best.
Celebrating Sensory Differences
Language shapes how children see themselves. The best approach is to reframe sensory traits as natural differences. Your child has texture preferences, not a texture problem. They have a sensitive taste system, not pickiness.
For many neurodiverse children, sensory differences come with gifts. Some children develop extraordinary focus when their sensory needs are met, or remarkable creativity solving sensory challenges. Many become deeply empathetic because they understand how others experience situations differently.
Sound sensitivity can accompany musical talent. Strong body awareness and agility may lead to athletic prowess. Visual sensitivity can fuel artistic creativity. Acute taste can translate to talent in cooking. There are many stories of successful people with sensory differences (artists, scientists, athletes, innovators) whose lives can inspire your children. Share their stories.
Encourage your child to describe their sensory experiences. Create space for them to explain how things feel, sound, or look. This builds self-awareness, communication skills, and pride in their unique perspective.
Build family routines that honor different sensory needs. Have quiet dinners as well as music-filled ones. Provide spaces tailored to individual preferences. Small rituals validate that different nervous systems need different things.
Teach siblings about sensory differences in age-appropriate ways. Help them understand that “different” does not mean “wrong.” Understanding family members can become advocates.
Your child will meet people who do not understand them. Equip them with simple explanations and confidence to state needs, e.g., “Loud sounds hurt my ears” or “I need to move to think.”
Model accepting your own sensory needs. If you feel overwhelmed, honor your needs without shame, whether by leaving an event or creating a sensory-friendly space at home. This teaches your child to do the same.
Children who understand their sensory profile build resilience: they identify triggers, use coping strategies, and communicate needs. They discover where they thrive and learn their experiences are valid. Daily validation teaches that their needs matter, shaping self-worth more than any specific accommodation. You will find your rhythm through trial and error. You already have what counts: awareness and commitment to respecting how nervous systems work.

Frequently Asked Questions
1. How do I know if my child has Sensory Processing Disorder (SPD)?
Every child has unique sensory preferences, but if their reactions interfere with daily life, learning, or relationships, it may be time to consult with a healthcare provider or occupational therapist experienced in sensory challenges.
2. Can a child have both sensory-seeking and sensory-avoiding behaviors?
Yes. Many children with SPD show mixed profiles—for example, they might seek out loud noises but avoid bright lights. It’s common for sensory needs to vary across different senses and situations.
3. Are sensory issues the same as autism or ADHD?
No, but sensory processing differences often occur alongside diagnoses like autism and ADHD. However, SPD can also exist independently of other conditions.
4. What strategies can help at home during sensory meltdowns?
Remain calm and focus on safety. Reduce sensory input (lights, sounds), provide comfort items or deep pressure if your child finds it soothing, and allow space for your child to regulate. Talk about what happened later, once everyone is calm.
5. Will my child outgrow their sensory sensitivities?
Sensory processing styles can change over time, especially with support and coping tools. Some children become more comfortable as they grow, while others will continue to benefit from strategies into adulthood. The goal is learning how to manage needs, not to “fix” who they are.

Blue Bird Day—the first therapeutic preschool and kindergarten program in the nation—fosters socialization, sensory regulation, and pre-academic learning in children ages 2-7 years. Our compassionate therapists practice a relationship-based and family-centered approach, provide parent training, and collaborate on goals and individualized intensive treatment plans for your child.
We believe in a collaborative and multi-disciplinary team approach to therapy. A team of occupational therapists, speech-language pathologists, dietitians, developmental therapists, behavioral therapists, physical therapists, and therapeutic assistants are created for each child to ensure child and family are fully supported and the best possible results are achieved.
Options for individualized, group and virtual therapy sessions are available as well.
Want to learn more or you have a specific question? Feel free to connect with us here!